Corneal refractive surgery is a popular alternative for correction of refractive errors. While successful at compensating spherical and cylindrical errors, we have shown that standard ablation profiles induce high amounts of (corneal and total) high order aberrations, particularly spherical aberration (Moreno-Barriuso 2001; Marcos et al. 2001), which result in a significant reduction of visual contrast sensitivity (Marcos et al. 2001). We have also investigated the optical changes induced by hyperopic LASIK (Llorente et al. 2004). In another study, we investigated whether cone directionality may change after a LASIK procedure (Marcos and Burns, 2009)
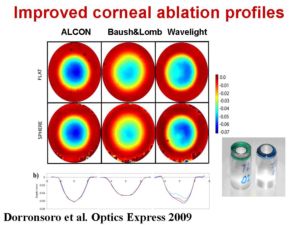
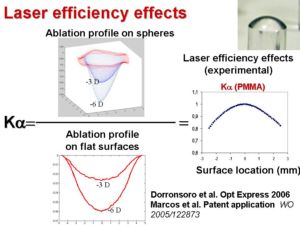
We study computationally (Marcos et al. JRS 2003; Cano et al. JOSA 2004) and experimentally (using plastic corneal models on plastic) the impact of the ablation profile and geometry-induced laser efficiency changes on optical performance, and propose methods for improvement of corneal ablation profiles (Dorronsoro et al. 2006; Patent WO 2005/122873). We have shown that in standard LASIK (and low fluence lasers) efficiency effects are a major cause for the increased asphericity (and spherical aberration) found in post-LASIK eyes. We have improved our model eyes in PMMA by providing them with new alignment capabilities, and a new material Filofocon A whose ablation properties we have investigated in detail (Dorronsoro et al. 2008). Using these new eye models in Filofocon A, we have evaluated the optical outcomes of three state-of-the art lasers provided with optimized ablation algorithms (Dorronsoro et al. 2009).
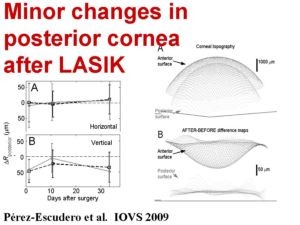
We also investigate the changes induced on the posterior corneal surface of the cornea in LASIK and address the contribution and impact of biomechanical changes in corneal stability. We have found that LASIK, unlile previously reported, does not produce a long term change in the posterior corneal shape. (Pérez-Escudero et al. 2009). The measurements were perfomed using a validated Scheimpflug imaging system.
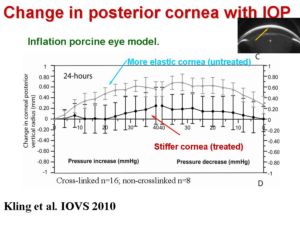 These studies suggest that corneal biomechanics may play a less relevant role in the outcomes of LASIK. However, there are recent corneal procedures that rely entirely in the modification of the corneal biomecahnical properties. One of these procedures is corneal collagen cross-linking with riboflavine. In this technique the cornea is stiffened when the cornea is exposed to UV light, that nominally creates bonds between collagen fibers. We have developed an in vitro inflation model to study corneal deformation upong varying pressure in normal eyes and eyes treated with cross-linking. We have demonstrated that the the procedure stiffens the cornea (increasing IOP produces less changes to the anterior and posterior corneal surface and corneal thickness), and therefore an increase in the Young modulus of the cornea (Kling et al. 2010).
These studies suggest that corneal biomechanics may play a less relevant role in the outcomes of LASIK. However, there are recent corneal procedures that rely entirely in the modification of the corneal biomecahnical properties. One of these procedures is corneal collagen cross-linking with riboflavine. In this technique the cornea is stiffened when the cornea is exposed to UV light, that nominally creates bonds between collagen fibers. We have developed an in vitro inflation model to study corneal deformation upong varying pressure in normal eyes and eyes treated with cross-linking. We have demonstrated that the the procedure stiffens the cornea (increasing IOP produces less changes to the anterior and posterior corneal surface and corneal thickness), and therefore an increase in the Young modulus of the cornea (Kling et al. 2010).
The use of new quantative anterior segment imaging techniques (such as Scheimpflug, and at higher resolution, OCT) opens new possibilities to the study of corneal changes following treatment and corneal biomechanical properties